Sciatica true or false
The Truth About Sciatica: Why Your "Sciatic Nerve Pain" Might Not Be Sciatica At All
If you've been diagnosed with sciatica or told you have sciatic nerve pain, you're not alone. Most days in my Madison massage therapy practice, I see clients who've been living with shooting pain down their leg, convinced their sciatic nerve is the culprit. Here's what might surprise you: nine out of ten times, the sciatic nerve isn't involved at all. After 26 years of practice and specialized training in Precision Neuromuscular Therapy (PNMT), I've learned that what most people call sciatica is actually something quite different—and often much easier to treat than true nerve involvement.
Understanding the real source of your hip pain, low back pain, or radicular pain is the first step toward finding lasting relief. In this post, I'll share what's really happening when you experience "sciatica," why the common treatment approaches often fail, and how proper assessment can get you back to living pain-free.
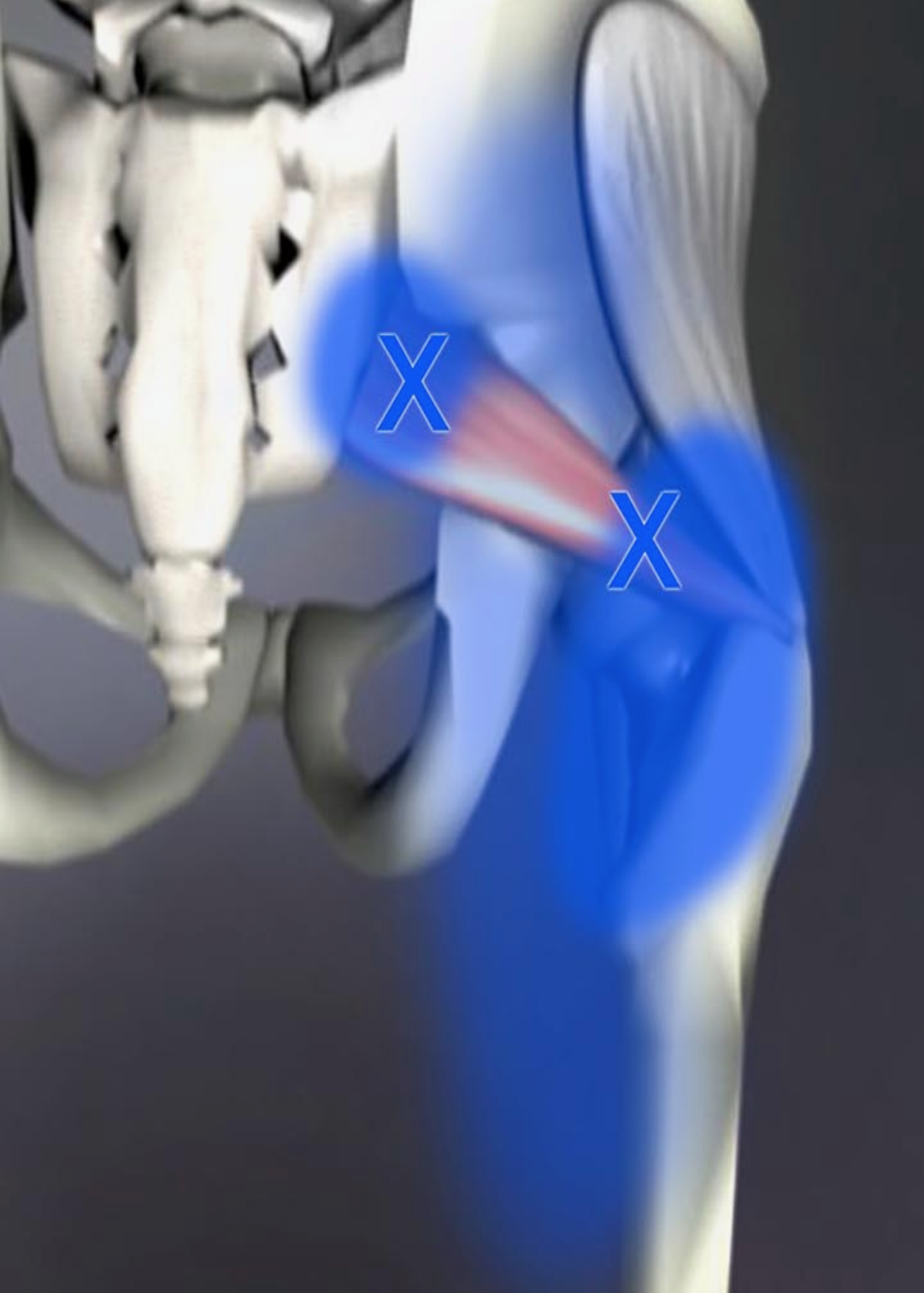
Gluteus Minimus pain referral pattern
Ready to Find Real Relief from Your "Sciatica"?
If you're tired of pain shooting down your leg and ready to discover what's actually causing it, let's work together to identify the root cause. With my PNMT training and 26 years of clinical experience, I can typically identify and begin treating the real source of your pain within just three sessions.
Book Your Appointment Now and start your journey toward lasting pain relief on Madison's west side.
Understanding True Sciatica vs. What You're Actually Experiencing
What Is the Sciatic Nerve?
The sciatic nerve is the largest nerve in your body, and understanding its anatomy helps explain why true sciatica is less common than you might think. This nerve originates in your lumbar spine and sacrum, specifically from nerve roots L4, L5, S1, S2, and S3. These nerve roots come together to form the sciatic nerve, which then travels down through your hip and leg, innervating the muscles in your lower extremities.
Why "Sciatica" Is Often Misdiagnosed
The term sciatica has become a catch-all diagnosis for any pain that travels from the hip or low back down the leg. In my practice in Madison WI , I see this presentation almost daily, and the vast majority of cases don't involve actual sciatic nerve compression or irritation. True radicular pain from nerve involvement has specific characteristics that differ significantly from muscular pain patterns, yet both can feel equally intense and debilitating to the person experiencing them.
The Real Culprits Behind Your Leg Pain
What most people experience as "sciatica" is actually referred pain from trigger points in the gluteal muscles, specifically the gluteus medius and gluteus minimus. These trigger points create pain patterns that mimic sciatic nerve distribution, sending discomfort down the side or back of the leg—sometimes all the way to the foot. The intensity can be just as severe as true nerve pain, which is why the confusion is so common, but the good news is that trigger point-related pain is typically much easier to treat than actual neurological involvement.
The Piriformis Connection: When the Sciatic Nerve Is Actually Involved
How the Piriformis Affects the Sciatic Nerve
When true sciatic nerve involvement occurs, the piriformis muscle is most frequently the culprit. This muscle is particularly problematic because the sciatic nerve passes directly under the piriformis muscle in most people, and in approximately 30 percent of the population, the nerve actually travels through the belly of the muscle itself. This anatomical variation makes some individuals more susceptible to piriformis-related sciatic nerve compression than others.
Presentation One: Direct Compression from a Shortened Piriformis
One of the most common scenarios I see involves one of the piriformis muscles (we have two, one on each side) tightening and shortening, which can put direct pressure on the sciatic nerve. This compression sends symptoms down the leg, often traveling all the way to the foot, and can create numbness, tingling, or sharp shooting pain. This presentation typically responds well to targeted manual therapy that releases the shortened muscle gives the pulled taught muscle some slack and takes pressure off the sciatic nerve.
Presentation Two: The Dangerous "Taut Band" Scenario
The second presentation is more complex and potentially problematic: one piriformis muscle shortens, often because of a leg position that's held for long periods and repeated frequently (think: sitting with your wallet in your back pocket, crossing the same leg repeatedly, or driving with one foot on the gas for hours). This shortened muscle then pulls the opposite piriformis muscle taut, stretching it tight over the sciatic nerve on that side. Here's where it gets tricky—the painful side is the one being pulled tight, not the shortened side, and the normal reaction to stretch into the pain actually makes the situation worse. The more you stretch a muscle that's already being pulled taut, the more pressure you create on the nerve beneath it.
Why Your Treatment Hasn't Worked (And What Will)
The Stretching Trap
If you've been stretching your piriformis or doing standard "sciatica stretches" without relief—or worse, with increased pain—you might be dealing with the taut band scenario I just described. Conventional wisdom says to stretch tight, painful muscles, but when a muscle is painful because it's being pulled tight from the other side, stretching it is exactly the wrong approach. This is where proper assessment becomes critical, and why working with someone trained in Precision Neuromuscular Therapy can make all the difference.
The Trigger Point Solution
For the nine out of ten cases where the issue is actually trigger points in the gluteus medius or minimus rather than true nerve involvement, treatment is remarkably straightforward. Using manual therapy techniques to release these trigger points typically provides rapid relief, often within the first few sessions. The key is accurate identification of which muscles are creating the referral pattern and addressing the underlying causes that created the trigger points in the first place—whether that's postural habits, movement patterns, or compensations from other injuries.
The PNMT Approach: Finding the Root Cause
My approach, grounded in Precision Neuromuscular Therapy training, focuses on isolating the actual root cause of your injury rather than just treating symptoms. Within three sessions, I can typically identify what's creating your pain and begin addressing it effectively. This might involve releasing trigger points, addressing muscular imbalances, correcting postural issues, or educating you about movement patterns that perpetuate the problem. The goal isn't just to make you feel better temporarily—it's to resolve the underlying issue so you can return to the activities you love without constant pain.
Recognizing the Difference: Do You Have True Sciatica?
Signs of Actual Nerve Involvement
True radicular pain from sciatic nerve compression typically presents with specific neurological symptoms beyond just pain. You might experience numbness or tingling that follows a specific nerve distribution, muscle weakness in the leg or foot, or changes in reflexes. If you're having difficulty lifting your foot (foot drop), significant weakness when standing on your toes or heels, or loss of bladder or bowel control, these are red flags that require immediate medical attention and indicate actual nerve compromise that may go beyond what massage therapy alone can address.
Characteristics of Trigger Point Referral
Trigger point-related pain, while it can be just as intense as nerve pain, typically has different characteristics. The pain may be deep and aching rather than sharp and electric, it often changes with position or movement in predictable ways, and it usually doesn't cause true numbness ( though it absolutely can). Pressure directly on the trigger point typically recreates or intensifies the referral pattern down the leg, which is a key diagnostic indicator.
Why Professional Assessment Matters
The distinction between these presentations matters tremendously for treatment success. Stretching exercises appropriate for one scenario can worsen another, and treatments that work beautifully for trigger points won't address true nerve compression. This is why working with a practitioner who can accurately differentiate between these conditions is so important. During your initial sessions, I'll perform specific assessments to determine exactly what's creating your symptoms and develop a treatment plan tailored to your specific situation.
Take the Next Step Toward Pain-Free Living
You don't have to live with shooting pain down your leg or avoid activities you love because of "sciatica." Whether you're dealing with true piriformis-related nerve compression or trigger point referral from your gluteal muscles, targeted manual therapy can help you find relief. After 26 years of practice here on Madison's west side, I've helped hundreds of clients overcome what they thought was permanent sciatic nerve pain.
The first step is accurate assessment. Once we understand what's actually causing your hip pain, low back pain, or radicular pain, we can create a treatment plan that addresses the root cause rather than just masking symptoms. Most clients begin to see improvement within the first three sessions as we identify and treat the real source of their discomfort.
Don't let another day go by accepting pain as your new normal. Book your appointment today and let's work together to discover what's really behind your "sciatica" and get you back to living without constant leg pain.